




 epilepsy (a disorder of the central nervous system characterized by loss of consciousness and convulsions)
epilepsy (a disorder of the central nervous system characterized by loss of consciousness and convulsions)Epilepsy (from the Ancient Greek ἐπιληψία epilēpsía) is a common chronic neurological disorder characterized by recurrent unprovoked seizures. These seizures are transient signs and/or symptoms of abnormal, excessive or synchronous neuronal activity in the brain. About 50 million people worldwide have epilepsy, with almost 90% of these people being in developing countries. Epilepsy is more likely to occur in young children, or people over the age of 65 years, however it can occur at any time. Epilepsy is usually controlled, but not cured, with medication, although surgery may be considered in difficult cases. However, over 30% of people with epilepsy do not have seizure control even with the best available medications. Not all epilepsy syndromes are lifelong – some forms are confined to particular stages of childhood. Epilepsy should not be understood as a single disorder, but rather as syndromic with vastly divergent symptoms but all involving episodic abnormal electrical activity in the brain
Epilepsy Overview
Epilepsy is a condition in which a person has recurrent seizures. A seizure is defined as an abnormal, disorderly discharging of the brain's nerve cells, resulting in a temporary disturbance of motor, sensory, or mental function.
There are many types of seizures, depending primarily on what part of the brain is involved. The term epilepsy says nothing about the type of seizure or cause of the seizure, only that the seizures happen again and again. A stricter definition of the term requires that the seizures have no known underlying cause. This may also be called primary or idiopathic epilepsyEpisodes of abnormal electrical activity within the brain result in seizures. The specific area of the brain affected by the abnormal electrical activity may result in a particular type of seizure.
If all areas of the brain are affected by the abnormal electrical activity, a generalized seizure may result. This means that consciousness is lost or impaired. Often all the person's arms and legs stiffen and then jerk rhythmically.
One seizure type may evolve into another during the course of the seizure. For example, a seizure may start as a partial, or focal, seizure, involving the face or arm. Then the muscular activity spreads to other areas of the body. In this way, the seizure becomes generalized.
Seizures caused by high fevers in children are not considered epilepsy. Also see children's seizures
There are many types of seizures, depending primarily on what part of the brain is involved. The term epilepsy says nothing about the type of seizure or cause of the seizure, only that the seizures happen again and again. A stricter definition of the term requires that the seizures have no known underlying cause. This may also be called primary or idiopathic epilepsyEpisodes of abnormal electrical activity within the brain result in seizures. The specific area of the brain affected by the abnormal electrical activity may result in a particular type of seizure.
If all areas of the brain are affected by the abnormal electrical activity, a generalized seizure may result. This means that consciousness is lost or impaired. Often all the person's arms and legs stiffen and then jerk rhythmically.
One seizure type may evolve into another during the course of the seizure. For example, a seizure may start as a partial, or focal, seizure, involving the face or arm. Then the muscular activity spreads to other areas of the body. In this way, the seizure becomes generalized.
Seizures caused by high fevers in children are not considered epilepsy. Also see children's seizures
TYPES OF Epilepsy
When a disorder is defined by a characteristic group of features that usually occur together, it is called a syndrome. These features may include symptoms, which are problems that the patient will notice. They also may include signs, which are things that the doctor will find during the examination or with laboratory tests. Doctors and other health care professionals often use syndromes to describe a patient's epilepsy
The type or types of seizures
The age at which the seizures begin
The causes of the seizures
Whether the seizures are inherited
The part of the brain involved
Factors that provoke seizures
How severe and how frequent the seizures are
A pattern of seizures by time of day
Certain patterns on the EEG, during seizures and between seizures
Other disorders in addition to seizures
The prospects for recovery or worsening
The age at which the seizures begin
The causes of the seizures
Whether the seizures are inherited
The part of the brain involved
Factors that provoke seizures
How severe and how frequent the seizures are
A pattern of seizures by time of day
Certain patterns on the EEG, during seizures and between seizures
Other disorders in addition to seizures
The prospects for recovery or worsening
Not every syndrome will be defined by all these features, but most syndromes will be defined by a number of them. Classifying a patient's epilepsy as belonging to a certain syndrome often provides information on what medications or other treatments will be most helpful. It also may help the doctor to predict whether the seizures will go into remission (lessen or disappear).
Partial seizure
Partial seizure
Partial seizures (also called focal seizures and localized seizures) are seizures which affect only a part of the brain at onset, and are split into two main categories; simple partial seizures and complex partial seizures
A simple partial seizure will often be a precursor to a larger seizure such as a complex partial seizure, or a tonic-clonic seizure. When this is the case, the simple partial seizure is usually called an aura.
Partial seizures are common in temporal lobe epilepsy
A simple partial seizure will often be a precursor to a larger seizure such as a complex partial seizure, or a tonic-clonic seizure. When this is the case, the simple partial seizure is usually called an aura.
Partial seizures are common in temporal lobe epilepsy
Generalized Seizures
A generalized seizure is a sudden change in consciousness, muscle control or behavior caused by abnormal activity on both sides of the brain. A generalized seizure is different from a partial (focal) seizure, which usually affects a small, localized area of the brain.
Seizures occur when the neurons in the brain suddenly increase activity, causing an electrical storm that can overwhelm the brain. This can result in various symptoms depending on the area of the brain affected. People who have a generalized seizure usually experience symptoms that affect their entire body, such as whole-body muscle contractions or a loss of consciousness.
Seizures occur when the neurons in the brain suddenly increase activity, causing an electrical storm that can overwhelm the brain. This can result in various symptoms depending on the area of the brain affected. People who have a generalized seizure usually experience symptoms that affect their entire body, such as whole-body muscle contractions or a loss of consciousness.
The most identifiable and traumatic type of generalized seizure is the tonic-clonic seizure, also known as grand mal seizures or convulsions. Many tonic-clonic seizures are isolated events and, although distressing to witness, rarely cause neurological damage.
Generalized seizures may be caused by chronic underlying medical conditions that may require treatment (e.g., epilepsy). Many generalized seizures have no known cause, making them difficult to prevent. In cases where the underlying cause is unknown, seizures can sometimes be controlled with medication.
Generalized seizures can rarely be treated with brain surgery because the abnormal neuron activity occurs in the entire brain. However, people with recurrent generalized seizures that are poorly controlled by medication may be suitable for a type of treatment called vagus nerve stimulation.
There are certain things bystanders can do (and not do) to prevent additional harm to a person having a generalized seizure. For example, nothing should be placed in a person’s mouth during a seizure, and restraint should not be used. It is recommended that bystanders clear the area of furniture and objects that may cause injury to the person having a seizure. Also, the person having the seizure should be gently rolled onto his or her side to prevent choking on vomit or mucus
Generalized seizures may be caused by chronic underlying medical conditions that may require treatment (e.g., epilepsy). Many generalized seizures have no known cause, making them difficult to prevent. In cases where the underlying cause is unknown, seizures can sometimes be controlled with medication.
Generalized seizures can rarely be treated with brain surgery because the abnormal neuron activity occurs in the entire brain. However, people with recurrent generalized seizures that are poorly controlled by medication may be suitable for a type of treatment called vagus nerve stimulation.
There are certain things bystanders can do (and not do) to prevent additional harm to a person having a generalized seizure. For example, nothing should be placed in a person’s mouth during a seizure, and restraint should not be used. It is recommended that bystanders clear the area of furniture and objects that may cause injury to the person having a seizure. Also, the person having the seizure should be gently rolled onto his or her side to prevent choking on vomit or mucus
Mechanisms of Action of Antiepileptic Drugs
Center for Treatment of Epilepsy and Migraine, Kielecka 25, 31-523 Kraków, 2Department of Neurology,
Neuropsychiatric Care Unit, Grunwaldzka 47, 25-736 Kielce, 3Department of Pathophysiology, Skubiszewski Medical
University, Jaczewskiego 8, 20-090 Lublin, 4Isotope Laboratory, Institute of Agricultural Medicine, Jaczewskiego 2,
20-950 Lublin, Poland
Center for Treatment of Epilepsy and Migraine, Kielecka 25, 31-523 Kraków, 2Department of Neurology,
Neuropsychiatric Care Unit, Grunwaldzka 47, 25-736 Kielce, 3Department of Pathophysiology, Skubiszewski Medical
University, Jaczewskiego 8, 20-090 Lublin, 4Isotope Laboratory, Institute of Agricultural Medicine, Jaczewskiego 2,
20-950 Lublin, Poland
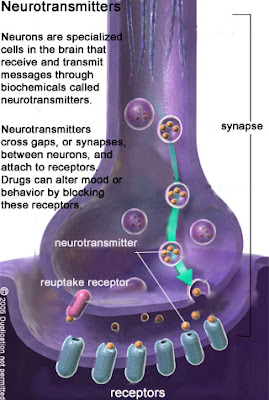
Abstract: g-Aminobutyric acid (GABA), one of the main inhibitory neurotransmitters in the brain, interacts with three types of receptors for GABA - GABAA, GABAB and GABAC. GABAA receptors, associated with binding sites for benzodiazepines and barbiturates in the form of a receptor complex, control opening of the chloride channel. When GABA binds to the receptor complex, the channel is opened and chloride anions enter the neuron, which is finally hyperpolarized. GABAB receptors are metabotropic, linked to a cascade of second messengers whilst the physiological meaning of ionotropic GABAC receptors, mainly located in the retina, is generally unknown. Novel antiepileptic drugs acting selectively through the GABA-ergic system are tiagabine and vigabatrin. The former inhibits neuronal and glial uptake of GABA whilst the latter increases the synaptic concentration of GABA by inhibition of GABA-aminotransferase. Gabapentin, designed as a precursor of GABA easily entering the brain, was shown to increase brain synaptic GABA. This antiepileptic drug also decreases influx of calcium ions into neurons
via a specific subunit of voltage-dependent calcium channels. Conventional antiepileptics generally inhibit sodium currents (carbamazepine, phenobarbital, phenytoin, valproate) or enhance GABA-ergic inhibition (benzodiazepines, phenobarbital, valproate). Ethosuximide, mainly controlling absences, reduces calcium currents via T-type calcium channels. Novel antiepileptic drugs, mainly associated with an inhibition of voltage-dependent
sodium channels are lamotrigine and oxcarbazepine. Since glutamate-mediated excitation is involved in the generation of seizure activity, some antiepileptics are targeting glutamatergic receptors – for instance, felbamate, phenobarbital, and topiramate. Besides, they also inhibit sodium currents. Zonisamide, apparently sharing this common mechanism, also reduces the concentration of free radicals. Novel antiepileptic drugs are better tolerated by epileptic patients and practically are devoid of important pharmacokinetic drug interactions.
via a specific subunit of voltage-dependent calcium channels. Conventional antiepileptics generally inhibit sodium currents (carbamazepine, phenobarbital, phenytoin, valproate) or enhance GABA-ergic inhibition (benzodiazepines, phenobarbital, valproate). Ethosuximide, mainly controlling absences, reduces calcium currents via T-type calcium channels. Novel antiepileptic drugs, mainly associated with an inhibition of voltage-dependent
sodium channels are lamotrigine and oxcarbazepine. Since glutamate-mediated excitation is involved in the generation of seizure activity, some antiepileptics are targeting glutamatergic receptors – for instance, felbamate, phenobarbital, and topiramate. Besides, they also inhibit sodium currents. Zonisamide, apparently sharing this common mechanism, also reduces the concentration of free radicals. Novel antiepileptic drugs are better tolerated by epileptic patients and practically are devoid of important pharmacokinetic drug interactions.
Key Words: Antiepileptic drugs, GABA, glutamate, ion channels, epilepsy.
RECEPTORS FOR GAMMA-AMINOBUTYRIC ACID
GABA may mediate its synaptic events through two types of receptors - ionotropic and metabotropic. Among ionotropic receptors associated with a chloride channel so
called GABAA and GABAC receptors are distinguished - metabotropic ones linked to the cascade of second intraneuronal messengers are GABAB receptors [4,5].
GABAA receptor complex consists of a number of binding sites for GABA itself, benzodiazepines, barbiturates, ethanol and picrotoxin which is a chloride channel blocker. When GABA binds to its recognition site on the GABAA receptor complex, an opening of the chloride channel occurs with the subsequent influx of chloride anions into a neuron, resulting in its hyperpolarization. Benzodiazepine derivatives (f.e.: diazepam, clonazepam) increase the frequency of the channel
openings whilst barbiturates (f.e.: phenobarbital) prolong the opening time of the channel. Both, benzodiazepines and barbiturates also enhance the affinity of GABAA receptors for
the neurotransmitter [4,5]. In contrast, binding GABA to the GABAB receptors results in the activation of phospholipase A-2 and the following synthesis of arachidonic acid fromphospholipids. Arachidonic acid via regulatory Gi proteins is likely to modulate the activity of adenyl cyclase and cyclic AMP levels. Through the GABAB receptors GABA affects
the release of other important for the neuronal activity neurotransmitters. GABAC receptors are mainly encountered in the retina and their physiological significance is a matter of dispute.
called GABAA and GABAC receptors are distinguished - metabotropic ones linked to the cascade of second intraneuronal messengers are GABAB receptors [4,5].
GABAA receptor complex consists of a number of binding sites for GABA itself, benzodiazepines, barbiturates, ethanol and picrotoxin which is a chloride channel blocker. When GABA binds to its recognition site on the GABAA receptor complex, an opening of the chloride channel occurs with the subsequent influx of chloride anions into a neuron, resulting in its hyperpolarization. Benzodiazepine derivatives (f.e.: diazepam, clonazepam) increase the frequency of the channel
openings whilst barbiturates (f.e.: phenobarbital) prolong the opening time of the channel. Both, benzodiazepines and barbiturates also enhance the affinity of GABAA receptors for
the neurotransmitter [4,5]. In contrast, binding GABA to the GABAB receptors results in the activation of phospholipase A-2 and the following synthesis of arachidonic acid fromphospholipids. Arachidonic acid via regulatory Gi proteins is likely to modulate the activity of adenyl cyclase and cyclic AMP levels. Through the GABAB receptors GABA affects
the release of other important for the neuronal activity neurotransmitters. GABAC receptors are mainly encountered in the retina and their physiological significance is a matter of dispute.
Occurrence of GABA in the central nervous system was demonstrated in 1950 and in the same decade GABA was shown to inhibit seizure activity after its direct cerebralapplication in dogs [7]. Certainly, this gave rise to the assumption that GABA-ergic inhibition may be an important factor in the suppression of seizure activity in epilepticpatients. GABA itself was not a good candidate for an antiepileptic drug since it very poorly entered the brain through the blood- brain barrier. Much attention was paid to a synthesis of GABA-ergic agonists, which would easily penetrate into the central nervous system. Such substances were soon available, for instance agents increasing brain GABA concentration due to the inhibition of GABA
metabolism: aminooxyacetic acid, g -acetylenic-GABA, g - vinyl-GABA or direct agonists, for example - muscimol. Actually, these substances were found to exert anticonvulsant
effects in a variety of experimental models of epilepsy. The initial enthusiasm was, however, not fully justified it soon would come out that muscimol displayed a proconvulsant activity in primates and humans [7]. This was understood in terms of an undesired effects of the diffuse
stimulation of GABAA receptors within the brain. Consequently, the subsequent search for GABA-ergic agents as potential antiepileptic drugs would focus on substances
indirectly enhancing GABA functions - via inhibition of its metabolism or reduction of its neuronal uptake. This strategy led to the discovery of potent anticonvulsant substances -
some of them are nowadays potent antiepileptic drugs
metabolism: aminooxyacetic acid, g -acetylenic-GABA, g - vinyl-GABA or direct agonists, for example - muscimol. Actually, these substances were found to exert anticonvulsant
effects in a variety of experimental models of epilepsy. The initial enthusiasm was, however, not fully justified it soon would come out that muscimol displayed a proconvulsant activity in primates and humans [7]. This was understood in terms of an undesired effects of the diffuse
stimulation of GABAA receptors within the brain. Consequently, the subsequent search for GABA-ergic agents as potential antiepileptic drugs would focus on substances
indirectly enhancing GABA functions - via inhibition of its metabolism or reduction of its neuronal uptake. This strategy led to the discovery of potent anticonvulsant substances -
some of them are nowadays potent antiepileptic drugs
ANTIEPILEPTIC DRUGS AND GABA-MEDIATED
INHIBITION
INHIBITION
Valproic acid in the form of sodium salt was introducedto the therapy of epilepsy in the early 60s. One of the most likely mechanisms responsible for its anticonvulsant activitymay be inhibition of its metabolic degradation resulting in the elevation of GABA level in the synaptic cleft [11]. However, there are also data indicating no correlation between the protective action of valproate and GABA increase - in fact, valproate clearly reduced seizure activity produced by the inhibitor of GABA synthesis, izoniazid, but did not restore the reduced GABA level [12]. As already mentioned, benzodiazepines (fe.: diazepam, clonazepam) and barbiturates (fe.: phenobarbital) potentiate GABA-mediated inhibition via the increase in the affinity of this inhibitory neurotransmitter to its recognition sites within the GABAA receptor complex and via the direct influence upon the channel which leads to the enhanced influx ofchloride anions into the neuron and subsequent hyperpolarization. Among novel antiepileptic drugs, tiagabine and
vigabatrin seem to express their anticonvulsant activity mainly through the GABA-ergic system. Other novel antiepileptics associated with GABA-mediated inhibition, which also share additional mechanisms of action, are: felbamate, gabapentin, and topiramate. Tiagabine and vigabatrin, and to a certain degree - gabapentin, may be considered as drugs whose development was associated with so called GABA hypothesis of epilepsy [13]. Vigabatrin is an irreversible inhibitor of GABA transaminase and its administration in animals or humans results in the 3-fold increase in synaptic GABA level [14-16]. Tiagabine inhibits neuronal and glial GABA uptake, leading thus to the enhancement and prolongation of GABA synaptic events [16,17]. The anticonvulsant activity of inhibitors of GABA uptake in various models of experimental epilepsy was shown much earlier but these substances did not cross the blood-brain barrier. This certainly disqualified their possible use as antiepileptic drugs [18]. Probably, as already mentioned, tiagabine and vigabatrin possess mechanisms of action closely related to GABA-mediated events in the synaptic cleft, in contrast to conventional and some novel antiepileptics which may block voltage-dependent sodium and calcium channels and impair glutamate-induced excitation. For instance, sodium channels are blocked by a variety of antiepileptic drugs, including benzodiazepines (at high concentrations), carbamazepine, felbamate, lamotrigine, oxcarbazepine, phenytoin, phenobarbital, topiramate, and valproate. Ethosuximide or zonisamide mainly affect T-type calcium channels, and felbamate, phenobarbital, and topiramate inhibit glutamate excitation [19]. Interestingly, gabapentin, a cyclic analogue of GABA, was designed as a GABA agonist easily passing the blood-brain barrier. However, no receptor activity of gabapentin was detected on the GABAA receptor complex, only increased GABA turnover being found in some rat brain regions [20,21]. Also, gabapentin was documented to increase GABA level in brains of epileptic patients [15]. It is evident now, that this antiepileptic drug binds to the specific unit of voltagedependent calcium channel and inhibits intraneuronal calcium ion flux from the extraneuronal space [22]. Two novel antiepileptic drugs, topiramate and felbamate, although possessing multiple mechanisms of action (see below), affect GABA-mediated inhibition as well. Specifically, the former seems to potentiate effects of endogenous GABA through a novel binding site on the GABAA receptor complex [21,23]. The latter enhanced GABA-dependent chloride currents in rat hippocampal neurons [24]. However, such effect in vitro was no longer evident in the absence of GABA and, moreover, felbamate was not shown to interact directly with the GABAA receptor complex [25]. Among conventional and novel.
vigabatrin seem to express their anticonvulsant activity mainly through the GABA-ergic system. Other novel antiepileptics associated with GABA-mediated inhibition, which also share additional mechanisms of action, are: felbamate, gabapentin, and topiramate. Tiagabine and vigabatrin, and to a certain degree - gabapentin, may be considered as drugs whose development was associated with so called GABA hypothesis of epilepsy [13]. Vigabatrin is an irreversible inhibitor of GABA transaminase and its administration in animals or humans results in the 3-fold increase in synaptic GABA level [14-16]. Tiagabine inhibits neuronal and glial GABA uptake, leading thus to the enhancement and prolongation of GABA synaptic events [16,17]. The anticonvulsant activity of inhibitors of GABA uptake in various models of experimental epilepsy was shown much earlier but these substances did not cross the blood-brain barrier. This certainly disqualified their possible use as antiepileptic drugs [18]. Probably, as already mentioned, tiagabine and vigabatrin possess mechanisms of action closely related to GABA-mediated events in the synaptic cleft, in contrast to conventional and some novel antiepileptics which may block voltage-dependent sodium and calcium channels and impair glutamate-induced excitation. For instance, sodium channels are blocked by a variety of antiepileptic drugs, including benzodiazepines (at high concentrations), carbamazepine, felbamate, lamotrigine, oxcarbazepine, phenytoin, phenobarbital, topiramate, and valproate. Ethosuximide or zonisamide mainly affect T-type calcium channels, and felbamate, phenobarbital, and topiramate inhibit glutamate excitation [19]. Interestingly, gabapentin, a cyclic analogue of GABA, was designed as a GABA agonist easily passing the blood-brain barrier. However, no receptor activity of gabapentin was detected on the GABAA receptor complex, only increased GABA turnover being found in some rat brain regions [20,21]. Also, gabapentin was documented to increase GABA level in brains of epileptic patients [15]. It is evident now, that this antiepileptic drug binds to the specific unit of voltagedependent calcium channel and inhibits intraneuronal calcium ion flux from the extraneuronal space [22]. Two novel antiepileptic drugs, topiramate and felbamate, although possessing multiple mechanisms of action (see below), affect GABA-mediated inhibition as well. Specifically, the former seems to potentiate effects of endogenous GABA through a novel binding site on the GABAA receptor complex [21,23]. The latter enhanced GABA-dependent chloride currents in rat hippocampal neurons [24]. However, such effect in vitro was no longer evident in the absence of GABA and, moreover, felbamate was not shown to interact directly with the GABAA receptor complex [25]. Among conventional and novel.

ReplyDeleteI did what a lot of people do when they want to know more about something. I googled it. I came across Dr ITUA herbal medicine on YouTube so many people thanking him about his good work. My son was epilepsy patent. I wasn’t running all over God’s creation with every man I could find but here I am. I have felt bad about myself for so many years now because of my son epilepsy status. I obviously still have some self-accepting to do but I want to thank Dr Itua for everything he have done for my Son ,after my son taking Dr Itua Herbal medicine my son was completely free from epilepsy within 2 weeks of usage, I think what you are doing is so admirable. you have helped me a lot! I want to definitely reach out to you and thank you for your amazing work. You are a good person, and an extremely talented man. You have helped millions with your herbs, and have really inspired me,and i pray you still continue doing the good work.you can also email him on drituaherbalcenter@gmail.com Or WhatsApp Number..+2348149277967 for help also if you are suffering from the list of disease below...Herpes Virus,Epilepsy,Genital Wart,Autism,Cold Sore,Hiv/Aids,Infertility(Finding it difficult to conceive) Or Man Infertility,